Cancer & Light
The Potential of Light to Improve Cancer Treatments
Cancer is a disease process in which cells undergo abnormal, uncontrolled cell division, leading to the growth of tumors or cell masses that can be fatal. Due to the prevalence of cancer, it's likely we all know someone who has been affected by cancer and has received the current standards of care, involving a broad range of therapies including chemotherapy, surgery, radiation therapy, and immunotherapy. While these treatment strategies can be highly effective, many cancers still lack treatment options. Further, these treatments have several limitations. For instance, chemotherapy simultaneously kills cancer cells and healthy cells, while surgery may increase risk of infection. The Dreaden Lab has been recently working to provide new treatment options for patients with poor prognoses by developing therapies that alter the immune system (immunotherapies) in safer and more effective ways.
One such technology functions by activating the immune system to target cancer cells using focused light. This technology capitalizes on signaling molecules made by cells, known as cytokines, which help to regulate the immune system and fight diseases (see Figure A). Recombinant cytokines hold great potential for cancer immunotherapy, evidenced by their ability to treat cancers with typically poor outcomes, such as metastatic melanoma. However, the clinical use of cytokines has declined in recent years due to challenges that include off-target toxicity and poor circulation time. Erik Dreaden, PhD, assistant professor of Biomedical Engineering & Pediatrics, and his team saw a need and a way to develop improved cytokines that have fewer side effects and improved circulation, eliminating the need for frequent, high dosing. To this end, Dreaden and his team developed a new class of cytokines that enable tissue-restricted activation of cytokines in response to external light exposure.
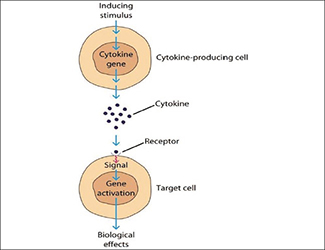
Mechanism of action of cytokines
Dreaden's technology shields the function of cytokines by binding stabilizing molecules that effectively act as an "off" switch and prevent cytokines from acting, and eliciting toxicity, throughout the body while simultaneously allowing them to circulate for longer periods. This is an existing protein engineering approach, but Dreaden's lab further refined this technique by adding an activation trigger: light. In response to light exposure of the appropriate wavelength, the stabilizing molecules are released, and the activity of the cytokine is turned back "on." Therefore, the Dreaden lab uses an "abiologic stimuli," light, to selectively activate certain cytokines and generate desired immune responses at discreet locations throughout the body. For example, turning "on" cytokines to produce an immune response to cancer within a tumor. Visible light can penetrate the transcutaneous layer (outer layer of skin) meaning this technology could be applied in melanoma, skin cancer, colorectal cancer, as well as head and neck cancer (throat), however, this presents a challenge for the treatment of deeper tissues. This is a current area of research for the Dreaden lab as they continue to devise new solutions for cancer treatment.
"Dreaden and his team use creative engineering approaches to overcoming the inherent limitations of biological systems" says Shweta Ghai, licensing associate in the Office of Technology Transfer. "Further, I believe this research will have an impact on improving the efficacy of current therapies in other disease areas" says Ghai.
Through this technology and the ability to precisely control cytokines, the Dreaden lab is gathering knowledge to understand the immune system and engineer new cancer treatments. Immunotherapies are continuously gaining interest as a cancer treatment strategy, and this technology has the potential to yet further enhance the effectiveness of this promising class of therapy.
Image courtesy of ResearchGate.
Techid: 19185
Read our technology brief